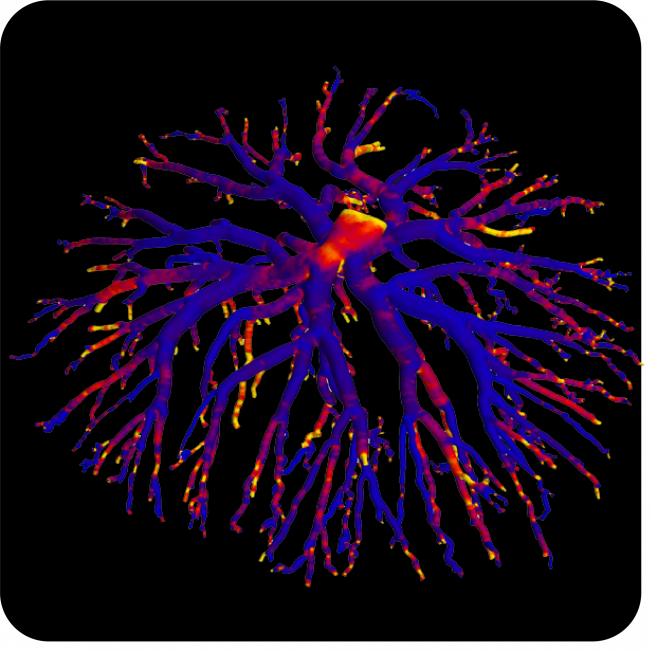
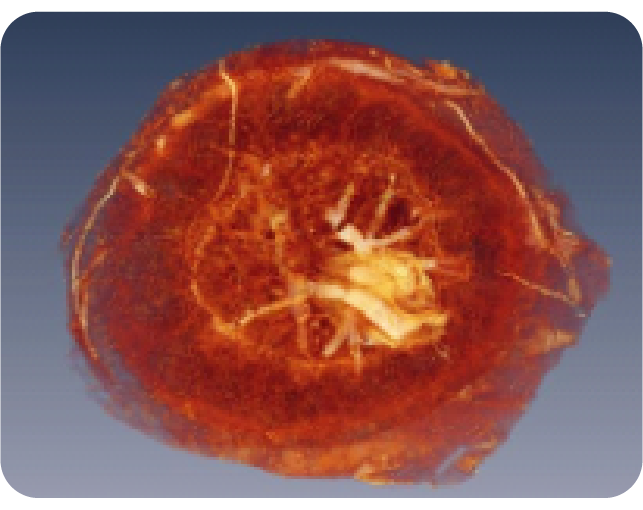
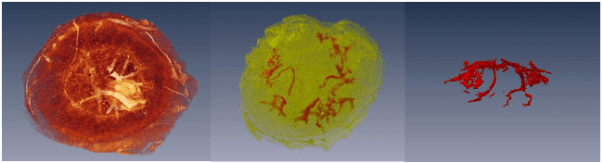
Understanding Feto-Placental Vasculature
Proper vascular development of the human placenta is crucial for meeting the metabolic needs of the developing fetus during pregnancy. Maternal environmental stressors such as malnutrition disrupt the elaboration of the feto-placental vasculature that, in turn, impacts on placental function and results in reduced fetal growth. The ramifications of this are not only on short-term foetal health but also on long-term health outcomes. Indeed, distortion in placental shape and size strongly associate with later adult health outcomes such as cardiovascular disease, obesity and cancer.
Read More