Impact of surgical lymph node removal
The impact of surgical lymph node removal on metastatic disease and the response to immunotherapy
Surgical resection of cancer remains the frontline therapy for millions of cancer patients every year, but disease recurrence after surgery is common with a relapse rate of around 45% for lung cancer. Relapse rates are expected to decline, with new immunotherapies producing extraordinary successes in several solid cancers. Immunotherapy administered after surgery could potentially ‘mop up’ small persisting cancer deposits that lead to disease recurrences. However, uninvolved (tumour-free) draining lymph nodes are the primary ‘factory’ for generating anti-cancer T cell responses; hence, should they be removed, subsequent immunotherapy may be negatively impacted. The aim of this project is to determine in murine models if the response of metastatic disease to immunotherapy is reduced following tumour lymph node resection.
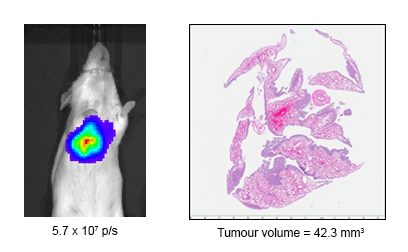
Dr Vanessa Fear of the School of Biomedical Sciences, at The University of Western Australia, is investigating if the response of metastatic disease to immunotherapy is reduced following tumour draining lymph node resection. To do this, the Tumour Immunology Group is using an AB1 Model of metastatic disease. Tumour progression is visualised using IVIS imaging and histology following resection to track the effectiveness of treatment regimes. Ultimately, the team will seek to determine the impact of lymph node removal at the time of tumour resection to subsequent immunotherapeutic outcomes.

Fig 1: IVIS imaging from AB1-HA tumour model. Mice received AB1-HA_LUC i.v. and lung tumour development monitored on the InVivo Imaging System (IVIS, Lumina II imager). At the imaged timepoints mice received intrapertioneal injections of luciferin (150µg/g) and tumour burden was measured on the IVIS in photons/sec (p/s). A, tumour progression day 14 to day 19.
The research project involves collaboration with the Centre for Microscopy, Characterisation and Analysis, the West Australian Node for the National Imaging Facility to image, visualise and characterise the development of lung metastatic disease using the IVIS Lumina II in vivo bioluminescence imager with the help of Living Image Software (Caliper Life Sciences).

Fig 2: IVIS imaging and histology from AB1-HA tumour model.Comparison of IVIS reading with lung H&E staining showing AB1-HA tumour from the same mouse. Tumour volume determined using FIJI software.
The team have completed preliminary studies determining a 55% metastatic disease onset after surgical resection of the primary tumour. Current investigations in tumour resection and lymph node resection indicate temporal changes in onset of metastatic disease compared to mice with intact lymph nodes.
Further investigations into the impact of lymph node resection on immunotherapy are underway. Future investigations will include other models including lung adenocarcinoma, melanoma, and breast cancer.
Collaborators
School of Medicine, the University of Western Australia
School of Biomedical Sciences, University of Western Australia
Centre for Microscopy, Characterisation and Analysis, the University of Western Australia
This story was contributed by the University of Western Australia. For more information, contact Dr Vanessa Fear or Diana Patalwala.