NIF investment builds understanding of Australia’s unique paleontological collections
A 105-million-year-old shark vertebrae fossil and a 4,000-year-old thylacine skull are amongst the first items to be scanned on NIF’s materials investment at the University of Western Australia (UWA), building a valuable digital collection of unique national artefacts with the Museum of Western Australia.
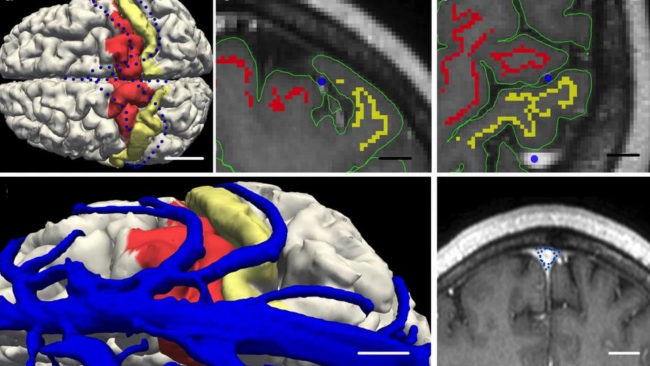
UWA NIF Fellow, Diana Patalwala said computed tomography was an invaluable tool for imaging materials providing high resolution 3D data, and preserving accurate anatomical information on the relative shape, size and location of different structures that would not be attainable by physical dissection.
“For each specimen, our materials-dedicated CT scanner takes approximately 1800–3000 x-ray images as the sample is rotated in the x-ray beam, at a level of resolution 100 times that of a typical medical CT scanner used on humans,” Ms Patalwala said.
“These images are then used to create a 3D model of the entire specimen, which is in essence a stack of virtual dissection slices that can be manipulated, rotated, and studied from every angle, revealing unprecedented details of the internal structure of the specimen.”
NIF is supporting the capture of this valuable data to create permanent digital records of specimen collections and enabling its reuse by multiple researchers to minimise duplication of efforts and resources.
Western Australian Museum Curator of Entomology, Collections and Research, Dr Nikolai Tartanic said the data captured could serve several different purposes.
“We’ve used scans to generate 3D models of items that can be printed and put on display. Sometimes these are scale models of minute organisms that are otherwise too small to observe and appreciate, other times we use 3D models to replace fragile or rare specimens,” Dr Tartanic said.
“The 3D datasets can also be shared with colleagues electronically, which in some cases replaces the need to send the physical specimen without putting the specimen at risk.”
Western Australian Museum Head of Earth and Planetary Sciences Dr Mikael Siversson said prior to the availability of this technology, some information about specimens could only be found by physical dissection, which could result in damage.
“In the old days, palaeontologists studying internal structures of vertebrate fossils would sometimes cut up the fossil slice-by-slice, and build a 3D model using clay,” Dr Siversson said.
“Printed 3D models enable palaeontologists to hands-on examine the morphology of primary type specimen without risking damaging the actual specimen.”
Scroll on to see some of the scans captured for the Museum’s collection.
Nullarbor Thylacine Skull sub-fossil: (Scan resolution: 105um; 185kV; 100uA)
Thylacinus cynocephalus (Tasmanian Tiger)
Murra-El-Elevyn Cave, Nullarbor

This subfossil skull from the Nullarbor was scanned in addition to a modern skull from Tasmania, enabling the team to capture data that can be used for morphometric (shape variation and comparison) studies.
This fossil is about 4,000 years old (carbon dated – 3,885 carbon years) and there’s a hole in the jaw where they took a sample for the carbon dating. It is thought to be a female, based on the size of the skull.
Shark vertebrae fossil: (Scan resolution: 56um; 200kV; 100uA)
Anacoracidae sp. (undescribed species of anacoracid shark)
Toolebuc Formation, Richmond, Queensland

This shark vertebra fossil is about 105 million years old (Albian Stage, Cretaceous Period), and belongs to a group of lamniform sharks called the anacoracids which were the Cretaceous ecological equivalents to modern whaler sharks.
Dr Siversson said the fossil represents a new species.
“It is exceptionally well preserved – anacoracid vertebrae are notoriously fragile – and this particular vertebra is surprisingly large considering the small size of anacoracid teeth in the same geological formation,” Dr Siversson said.
The team suspects this species was a plankton feeder, and based on its size, the animal would have been about four metres in length.
Aplysinopsis sponge: (Scan resolution: 91um; 850V; 250uA)

This species of sponge belongs to the order Dictyoceratida, which are sponges with spongin fibres. Some of them incorporate sand granules in their fibres, and small crustanceans are often found inside the sponge cavities.
Scanning revealed this sponge had several brittle stars living within it.
Echinodictyum Clathroides: (Scan resolution: 121um; 180kV; 100uA)


This species of sponge was first discovered in Shark Bay area, making its location a type locality. The sponge has three different spicules found in its fibres, some densely covered with spines.
Amber resin (Scan resolution: 78um; 190kV; 100uA)

These are specimens of amber-like natural resin of paleobotanical origin collected from WA beaches. The ultimate origin of this amber-like resin is likely South East Asia and it is thought these samples may have floated down to Rottnest Island where they were collected all the way from Indonesia.
Chemical analysis of similar amber found on Cape York in Queensland identified that it was produced by the Dipterocarpaceae, a family of lowland tropical rainforest trees.
Dr Tatarnic said the research team were looking for trapped insects using the CT scanning, but unfortunately did not find any.
“Scans of amber can detect the presence of now extinct insects. These may be new to science, or they may help us reconstruct past ecosystems, or identify from where the piece of amber originates,” Dr Tatarnic said.
The Nikon XT H 225 ST CT scanner was delivered to UWA in 2022 and is funded by National Imaging Facility, enabled by the National Collaborative Research Infrastructure Strategy, with the Government of Western Australia and supporters of the Western Australia National Imaging Facility.
For further information, contact NIF Facility Fellow, Diana Patalwala diana.patalwala@uwa.edu.au.