Brain research supercharged by new ‘control panel’ accessible worldwide
The flood of data from brain research worldwide has now been channelled into an easy-to-use, open-access processing tool built to supercharge our understanding of the human brain.
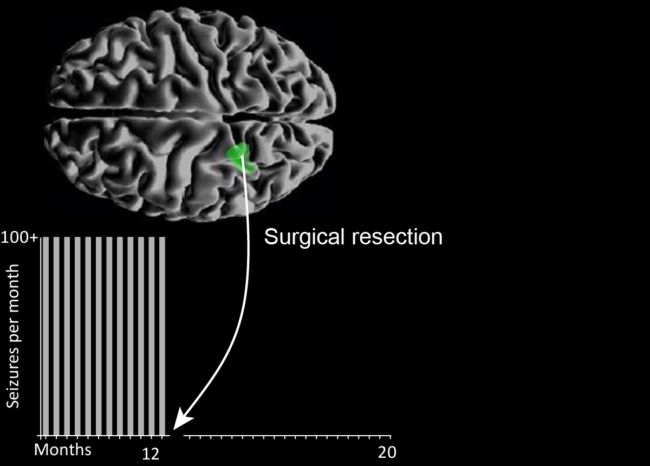
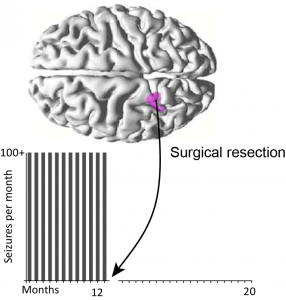
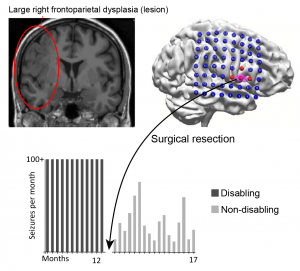
Neurodesk – a platform for processing, analysing and sharing massive datasets – has solved critical issues in the search for answers about brain disorders and diseases such as epilepsy, dementia, schizophrenia and traumatic brain injury. Neuroimaging data comes from modalities such as MRI, PET and MEG/EEG scans.
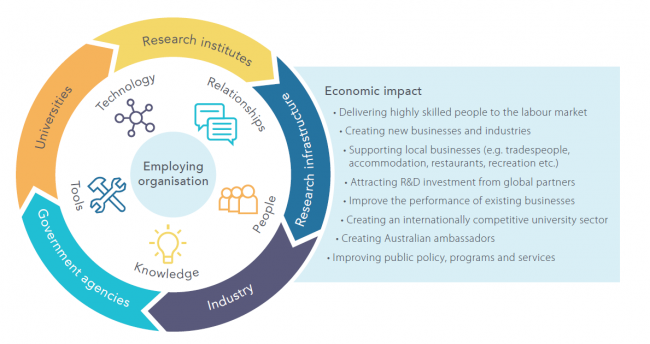
Neurodesk was proposed at, led by and supported by National Imaging Facility partners including the University of Queensland, Swinburne University of Technology, and the Australian Imaging Service through University of Sydney.
“It has removed a significant bottleneck that has hindered our ability to explore the complexities of the human brain, streamlining the processing of vast amounts of neuroimaging data,” says Dr Steffen Bollmann, project lead at the University of Queensland.
[Image: Members of the Neurodesk team, Aswin Narayanan, Thuy Dao, Dr Steffen Bollmann. Image credit: Dr Nicholas Hamilton.]
Both individual people and society stand to benefit: unravelling the brain’s mysteries helps us find cures for debilitating brain disorders, relieve people of the pain of untreated mental health issues and its societal cost, develop personalised medical treatments, inform public health policies, and understand human behaviour.
Neurodesk is like the ultimate, seamless sci-fi control panel. Accessible through a user-friendly browser interface, it works across operating systems, pulling together different neuroimaging programs that run in all different ways, and is able to run giant research projects or small ones with its seamless access to computing power.
Dr Bollmann sees Neurodesk’s accessibility as a leap forward in democratising neuroscience tools: “It empowers researchers worldwide to use open-source neuroimaging tools effectively and focus on their research questions, rather than grappling with technical obstacles.”
“It is difficult to overstate how much benefit Neurodesk provides to our facility,” says Dr Tim Rosenow, NIF Facility Fellow and Neurodesk user at UWA’s Centre for Microscopy Characterisation and Analysis. “Researchers no longer need to be experienced in IT to perform their analyses, because software, dependencies, and conflicts are already handled.”
However, the most important aim of Neurodesk’s creators was reproducibility: the process of other researchers replicating studies to check results and build a foundation of reliable scientific knowledge. The platform contains techniques that enable researchers to accurately replicate other teams’ analyses.
Scientists can even share and publish their analyses, which can significantly reduce time and effort for collaboration and creating new knowledge. They can then tackle bigger neuroscience questions and analyse larger datasets.
The ability to handle huge amounts of data is crucial, moving forward in brain research. Neurodesk gives researchers access to supercomputers and cloud computing to process neuroimaging data efficiently, letting them work with ‘biobanks’ of data (for instance, the UK Biobank holds imaging data from 50,000+ people).
“By simplifying neuroimaging, fostering collaboration and empowering scientists to handle huge datasets, this breakthrough not only advances our understanding of the healthy human brain, but also sheds light on the intricacies of various brain disorders,” says Dr Bollmann, “promising improved diagnostics and treatments in the future.”
Read the new paper published in Nature Methods here.