Catching the wave
Catching the wave: non-invasive MEG/EEG for epilepsy seizure localisation
Over 250,000 Australians currently live with epilepsy, a chronic disorder of the brain. In addition to significant social, physical and psychological consequences, epilepsy is linked with an increased risk of death compared to the general population. Up to 70% of epilepsy cases may be controlled through lifestyle and medication; however, many patients are unable to be treated using conservative measures. A major clinical problem, drug-refractory focal epilepsy may require aggressive treatments, including surgery, to resect a portion of the brain.
The localisation of the epileptogenic zone (the portion of the brain requiring resection to reduce seizures) is typically carried out clinically using magnetic resonance imaging (MRI). In many cases, no abnormalities are detected, requiring further investigation. Surgeons may also use invasive surgically implanted electrodes (intracranial electrode depth or grid, or ICEEG) for seizure source localisation, increasing the risk to the patient. A lower risk option is further functional imaging with positron emission tomography (PET), single-photon emission computed tomography (SPECT), and simultaneous electroencephalography functional MRI (EEG-fMRI). Unfortunately, many of these modalities lack temporal resolution to distinguish seizure onset.

“Catching the earliest wave, the earliest is key”
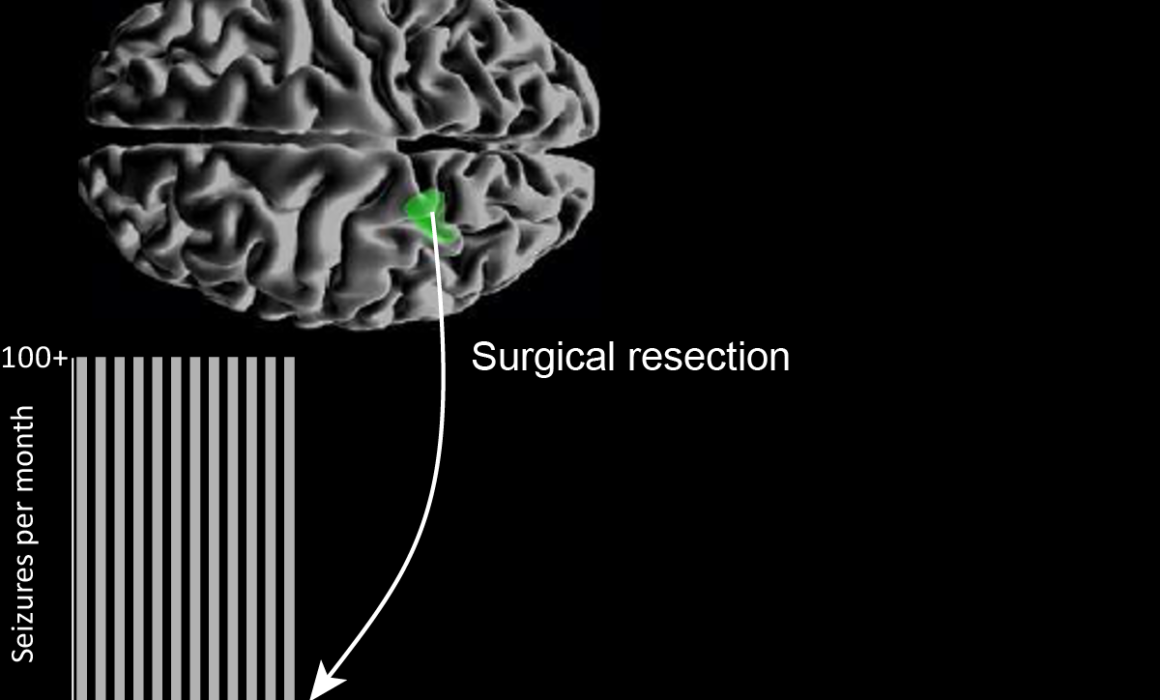
Representation of MEG (green) and EEG (blue) overlays.
Magnetoencephalography (MEG) and electroencephalography (EEG) offer a non-invasive method to detect rapidly evolving brain wave spikes and seizures at millisecond temporal resolution. A/Prof Chris Plummer and team, Mr Simon J. Vogrin, Dr William P. Woods, A/Prof Michael A. Murphy, Prof Mark J. Cook, and Prof David T.J. Liley, have developed a world-class multimodal technique for non-invasive source localisation and epileptogenic zone characterisation. The method (using co-acquired MEG and high-density EEG) has already improved the surgical treatment of medically refractory epilepsy, with clinical validity demonstrated in a key 2019 publication.
The team utilised the world-class MEG at the SUT NIF Node together with the expertise of NIF Facility Fellow Dr Will Woods to look at the efficacy of concurrent HDEEG (High-Density EEG > 64 electrodes) and MEG for identifying the epileptogenic zone. Ninety-six patients have been involved in the long-term prospective study. Seventy-one patients were MRI negative and twenty-five MRI positive with either complex lesions or multiple lesions. More than five years’ data collection in collaboration with neurologists and medical scientists found that the combined method was able to detect interictal spike discharges (between seizures) at early, mid and late-phase as well as ictal discharges (during seizures). The earliest resolvable localisation by either EEG or MEG was determined to be the most suitable site for surgical resection.
“We find that for most cases, modelling either the mid-upswing or the later peak (still common practice) results in mislocalization of the cortical generator (and the putative Epileptogenic Zone) due to the effects of discharge propagation across the cortical surface. We look for the earliest feature from the discharge; sometimes it appears first in the Magnetometer, sometimes it is first in one of the Gradiometers, and sometimes it is first in the HDEEG. For a given patient, there is typically a dominant leading modality, but the modality that leads in time will vary from patient to patient. This is fundamentally the reason for recording both. Otherwise, you risk having half the story before diving into invasive investigations.” – A/Prof Plummer
To date, successful source localisation has guided successful surgical outcomes in 25 patients, 8 of whom were spared invasive intracranial monitoring due to this method. Many of the over 100 studies performed are yet to progress to surgery, underpinning the latent potential of yet to be followed complete surgical workup and seizure-freedom outcomes following surgical therapy.
“Accurate, non-invasive localisation with this method will reduce the medical burden of invasive intracranial electrode monitoring by reducing the number of invasive electrodes required and, in some cases, remove the need for these in the first place to allow the patient to proceed directly to potentially curative surgery.” – A/Prof Plummer
This work intends to revolutionise epilepsy management in Australia, with data from a larger and more diverse cohort expected to provide evidence for a Medicare rebate to facilitate the accessibility of this technique for Australians.
Success stories:
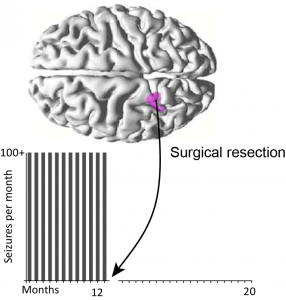
From 500 seizures per month to none; MEG/EEG guided surgical resection success
A young man with a five-year history of disabling seizures was suffering up to 500 seizures per month; his schooling was disrupted, and all the standard non-invasive tests gave conflicting results. Surgical resection was performed correlating with the earliest EMSL result. The patient is now seizure-free and on minimal medication following surgery.
A 10-year old child had a four-year history of left leg motor-sensory events, up to 200 times per day, leading to falls. PET and MRI suggested localisation of seizures in the right superior frontal gyrus and the right paracentral lobule, while EMSL results showed seizure onset further to the rear at the precuneus. Surgical resection of the paracentral lobule and superior frontal gyrus did not relieve the seizures seen by ICEEG during surgery. Further exploration revealed a second pocket of dysplasia in line with the EMSL result, resection of which normalised the ICEEG and relieved the patient of seizures.
A 36-year-old patient presented with speech-arresting complex partial turns with a typical MRI result. Their surgical plan was altered to include a hippocampal depth electrode, where seizures were found to start by MEG. Standard anteromesial temporal lobectomy revealed a cortical dysplasia involving the entorhinal cortex. The patient is now seizure-free and works as a speech therapist.
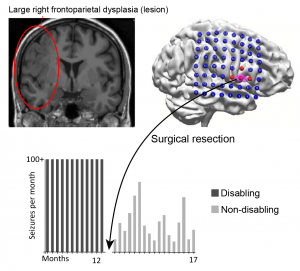
Recovering day to day activities without disturbing the complex dysplasia
A 36-year old mother of two young children suffered a 33-year history of multiple-daily disabling motor seizures. She was denied surgery due to a complex lesion seen by MRI (frontoparietal dysplasia). EMSL captured the seizure onset, targeting surgical resection without interfering with the bulk of the lesion. The patient is now on reduced medication and experiences only brief non-disabling focal seizures. She states that she “has her life back”.
You can learn more about epilepsy here or by speaking to your GP. This work was contributed by St Vincent’s Hospital, Swinburne University of Technology, and the University of Melbourne. For more information, please contact Dr Will Woods.