World-leading imaging technology reveals insights into cancer treatment for children with Down Syndrome
World-leading imaging technology reveals insights into cancer treatment for children with Down Syndrome.
The National Imaging Facility (NIF) continues to enable imaging science to unlock major health challenges with break-through research coming out of the South Australian Health and Medical Research Institute (SAHMRI).
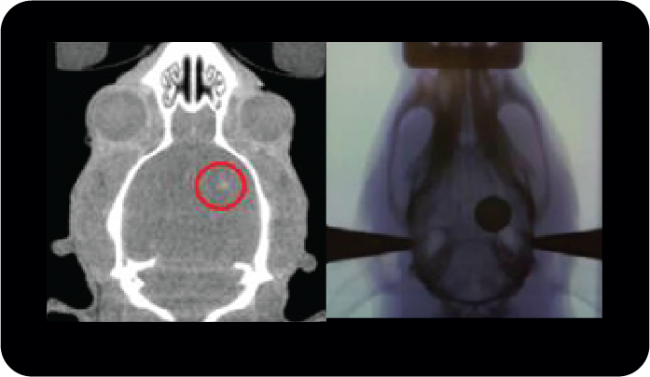
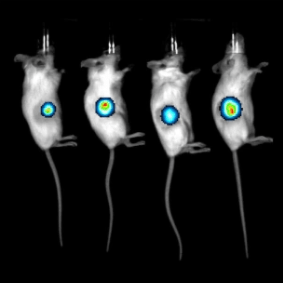
Leading-edge research using bioluminescent imaging conducted at the NIF’s South Australian Node has provided critical insight into the development of cancer in children with Down Syndrome.
Scientists from SAHMRI have identified an epigenetic regulator, HMGN1, on chromosome 21 that cooperates with a high-risk gene fusion to give rise to acute lymphoblastic leukaemia (ALL) in paediatric patients with Down Syndrome.
Children with Down Syndrome are 20 times more prone to developing leukaemia, and are more susceptible to experiencing additional side effects from chemotherapy. In addition to these statistics, 60% of children with Down Syndrome ALL harbour this high-risk gene fusion, and all have high expression of chromosome 21 genes.
SAHMRI’s findings suggest HMGN1 is a potential target for a precision treatment approach in Down Syndrome ALL. The outcomes from this study present an opportunity to reduce exposure in patients to the toxic side effects of chemotherapy and improve survival outcomes for children with Down Syndrome ALL.
NIF Node Co-Director, Dr Chris Christou praised the work of the SAHMRI team, including Prof Deborah L White and Dr Elyse Page and congratulated them on the findings which present potentially life-saving data.
“These dedicated and highly-skilled scientists have demonstrated the critical role imaging has in responding to major health challenges,” Dr Christou said.
“I congratulate them on this vital discovery and look forward to updates on their continued work progressing their research to improve the lives of children with Down Syndrome.”
You can read a detailed post about the study here.
For more information, contact Wick Lakshantha, Imaging Scientist and National Imaging Facility Fellow, SAHMRI.