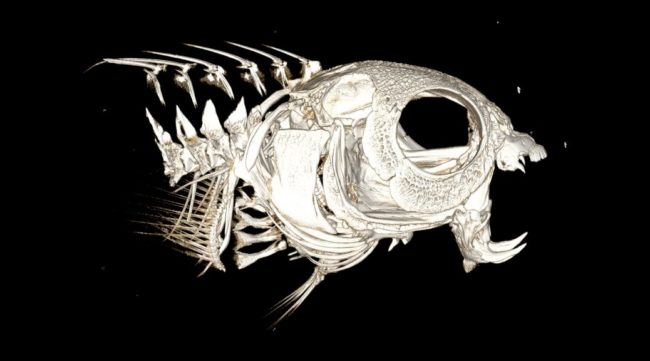
New diagnostic strategies to determine cardiovascular risk
Despite significant advances in diagnostic and therapeutic technologies, cardiovascular disease (CVD) remains the global leading cause of death, accounting for 17.3 million deaths per year, and is expected to grow to more than 23.6 million by 2030. Currently, the prevention of MI and stroke is limited due to the lack of sensitive imaging methods. Those available usually involve invasive procedures such as coronary angiograms, which are potentially associated with complications, including death caused by MI or bleeding. Hence, there is a great need for new diagnostic strategies to determine whether the individual patient is at risk of MI or stroke, which then would allow for effective and early preventative treatment and improved clinical outcome.
This project is a multicentre collaboration led by the University of Queensland (UQ), Australian Institute for Bioengineering and Nanotechnology (AIBN), including the Queensland nodes of the National Imaging Facility and Australian National Fabrication Facility, Monash University, Baker IDI Heart and Diabetes Institute and the SooChow University. Together this project developed novel molecular imaging nanoparticles to enhance for MRI detection of activated platelets which is associated with unstable vulnerable atherosclerotic plaques.
A complete description of the project, including the particles and imaging methods, is available via the a publication in Biomaterials journal.