Wendy Randall was working as a regional nurse when she had her first seizure at the age of 42. Despite trying a variety of medications over the next 11 years, she continued to experience seizures, sometimes daily.
Then in 2024, she discovered the Australian Epilepsy Project (AEP), and through her neurologist had a sequence of MRI scans that revealed temporal encephaloceles (extrusions of brain tissue through her skull, caused at birth). This condition is potentially curable, and Wendy is now undergoing monitoring and further investigations for possible surgery.
Wendy’s story and others were included in the AEP’s recently released 2025 AEP Impact Report. The AEP was established with $30 million of Australian Government funding via the Medical Research Future Fund in 2021, with a mission to change the lives of people living with epilepsy.
The AEP aims to use the data it collects using precision medicine to overcome three main problems:
- the uncertainty of diagnosis, progression of disease and treatment for the 250,000 Australians currently living with epilepsy
- the lack of access to diagnostics and treatments, especially for those living in regional areas like Wendy
- the costs to individuals and the economy (estimated at $12.3 billion per year) from healthcare costs and lost productivity.
The AEP now has seven MRI scanning sites across five states as part of a national network to provide epilepsy patients with access to advanced diagnostic testing that was otherwise only accessible to a small number of patients each year.
These scanning sites are part of NIF’s national advanced human imaging network, which provides advanced imaging capabilities, computational techniques and informatics.
Through NIF facilities, AEP participants like Wendy undergo comprehensive, advanced MRI protocols that are designed to detect epilepsy-related changes to the brain’s anatomy and cognitive functioning, such as memory and language.
So far, 1400 patients have been referred to the AEP by the 143 neurologists registered with the AEP. This means patients across the country, including in regional and remote Australia, have access to the gold-standard care usually only available to those with city postcodes. The AEP has given me “the opportunity to take part in a thorough process to establish causation and diagnosis,” said one participant from a regional area.
This participation level has resulted in almost 900 AEP reports being delivered to patients through their neurologists across Australia. These detailed reports provide the basis for better decision-making about the best possible treatment.
For some patients, this means they can potentially receive surgery that will give them freedom from seizures. And this surgery can potentially happen within two years of diagnosis, rather than was typical for Wendy and many patients like her who have had to wait for up to 20 years from diagnosis to surgery.
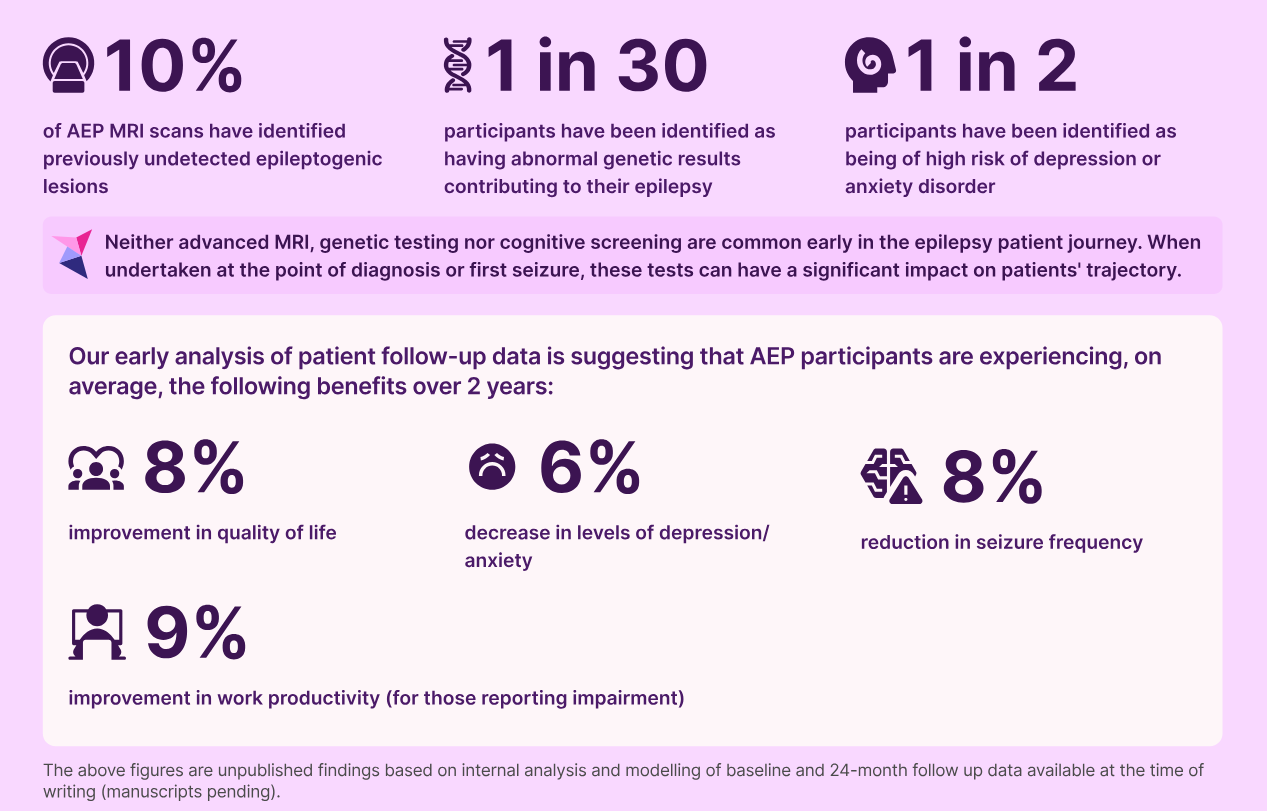
The 2025 AEP Impact Report demonstrates the help patients are gaining from their participation. Ten per cent of MRI scans have identified previously hidden seizure-inducing brain lesions.
Participating AEP patients also report an 8 per cent improvement in their quality of life, a 6 per cent decrease in their level of depression or anxiety, an 8 per cent reduction in seizure frequency, and a 9 per cent improvement in work productivity.
“Everybody else gave up on me, especially my doctors. One day I found the AEP [and] it’s been a magical experience. [They] found things that could be the true cause of my seizures. I am so glad I reached out to them,” said Wendy Randall (quoted in the 2025 AEP Impact Report).
NIF is proud to support the AEP through its national network of Nodes and expertise.
Images are courtesy of the AEP’s impact report 2025.