3D printed devices to treat traumatic pelvic fractures
3D printing is increasingly being used in the healthcare industry to customise medical devices to meet patient-specific needs. Currently, device manufacture is lengthy, limiting the application of customised medical devices. The treatment of traumatic injuries requires intervention as quickly as possible, preferably within days post-injury.
This collaborative research project between the Dept. of Biomedical Engineering at the University of Melbourne and the Dept. of Orthopaedics at the Royal Melbourne Hospital aims to assess the feasibility of 3D printing fracture plates to treat traumatic fractures and speed up the production of devices at the point-of-care for a patient. By performing a proof-of-concept experiment on a set of cadaveric pelvis, Dr Dale Robinson and team are evaluating each phase of the 3D printing workflow. Once implanted, a series of computational models and biomechanical experiments will be used to assess whether the 3D printed fracture plate offers an improvement over a traditionally mass-manufactured plate. Paramount to designing customised implants, the anatomy of each pelvis is being characterised using the University of Melbourne’s NIF Node CT with input from PET/CT Facility Fellow Rob Williams and radiographer Rebecca Glarin. After implantation of the fracture plate, CT may assess the effectiveness of the device in terms of stabilising and reducing the fracture.
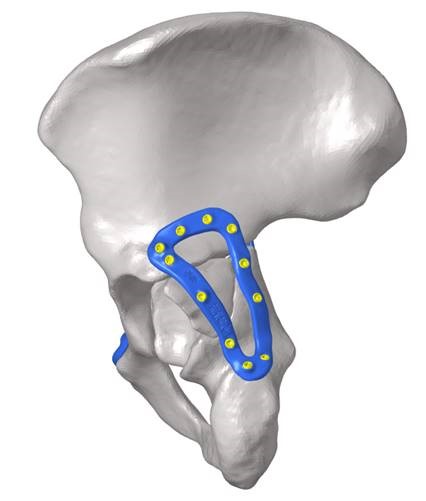
3D reconstruction of a fractured human pelvis with a custom 3D printed device simulated in blue to promote appropriate healing.
To date, the project has conducted some scans and used this data for preliminary printing of implants. Plates were designed and printed in collaboration of researchers at Johnson and Johnson and the University of Melbourne. The initial study used 3D printed medical-grade titanium and 3D rendering from the NIF facility CT. In developing this method, iterative reconstruction with maximal overlap to printing was used to be consistent with typical medical CT. This was done while still using radiation dosimetry within standard limits.
This project has the potential to improve patient outcomes by enhancing surgical intervention durability, reducing the duration and number of surgeries, and reducing the risk of life-threatening surgical complications (such as pulmonary embolism and infection) through reduced bedtime. Consequently, the effective implementation of customised 3D printed medical devices is expected to reduce healthcare costs through shorter hospital stays and reduced number of surgical interventions.
This story was contributed by the Department of Biomedical Engineering and the Melbourne Brain Centre Imaging Unit at the University of Melbourne, and Johnson & Johnson. For further information, please contact Rob Williams.