Local Connectivity Networks Disrupted by Sports-Related Concussion
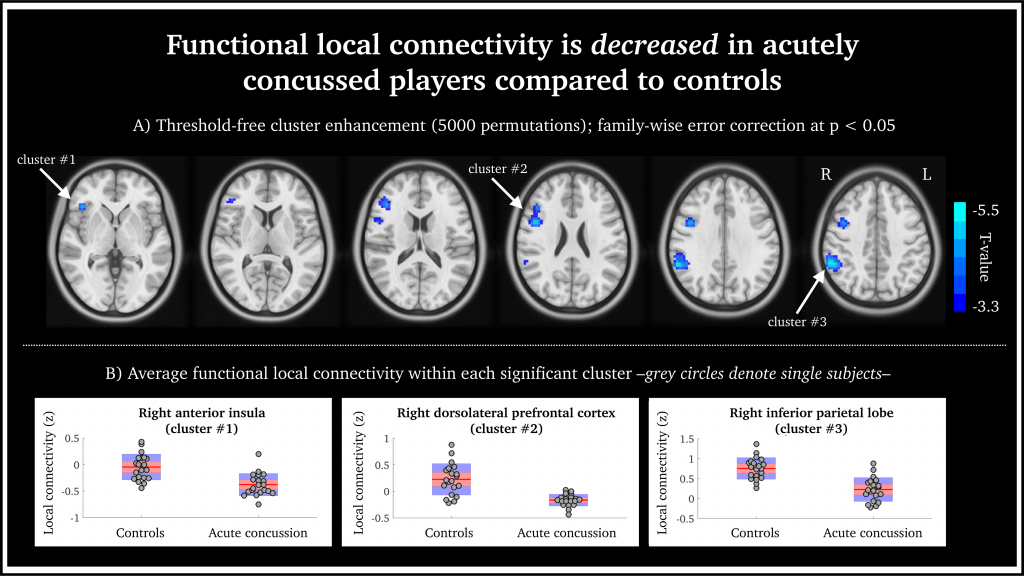
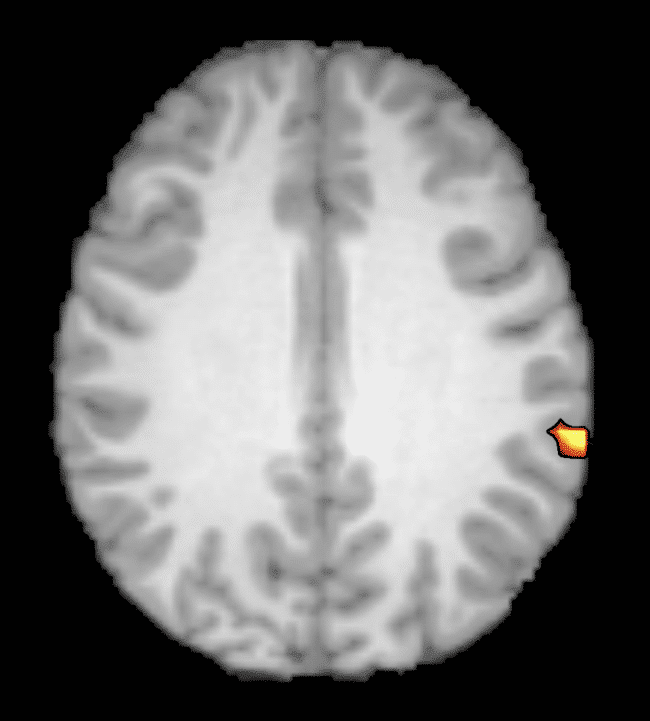
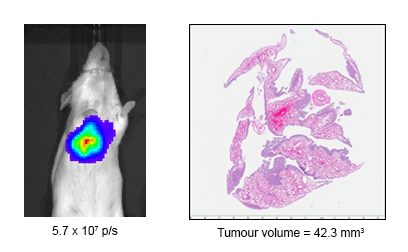
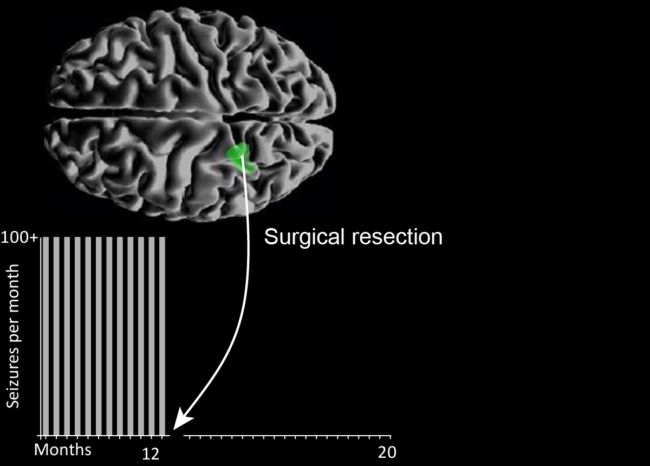
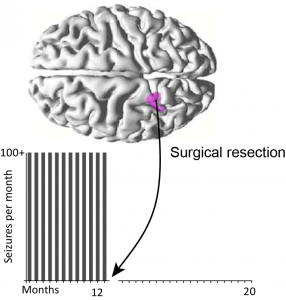
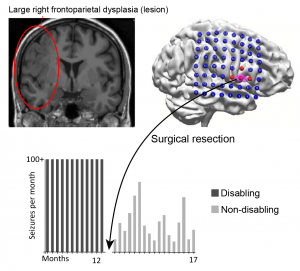
Functional local connectivity is decreased in acutely concussed players compared to controls. (a) Statistically significant brain regions at family-wise error rate p < 0.05; 5000 permutations using threshold-free cluster enhancement. Cool-scaled color bar denotes the magnitude of voxel t-values. (b) Individual-level z-normalized fMRI local connectivity values where each grey circle denotes an individual subject; red line is the group mean; red shaded area is the 95th percentile of the mean value; and blue shaded area is one standard deviation from the mean.
Head injuries, including concussion, are taken very seriously in sporting professions. To date, making an accurate diagnosis of acute concussion has been made difficult by the lack of a reliable direct biomarker for injury and recovery. This diagnostic gap can lead to unknown recovery periods and potentially long-term impacts for athletes.
Researchers at the Florey Institute of Neuroscience and Mental Health set out to understand functional brain changes in professional players in the Australian Football League who had been diagnosed with acute sport-related concussion.
The world-first study, published in the Journal of Concussion, utilised NIF infrastructure, the 3T Trio and Skyra MRI scanners, and NIF expertise, Facility Fellows Shawna Farquharson and David Abbott.
Functional MRI (fMRI) was undertaken to assess functional connectivity alongside anatomical imaging. Although no anatomical damage was observed, the authors described a decreased intrinsic fMRI connectivity within the right frontoparietal regions in acutely concussed footballers. In other words, all 20 concussed athletes showed reduced activity in parts of the brain responsible for executive function, working memory and switching tasks.
“By looking at how the different parts of the brain talk to each other, we can see how these three brain networks are affected, and these changes may help explain the symptoms we see in concussed players.” – Dr Mangor Pedersen, study co-author, from the Florey Institute of Neuroscience and Mental Health.
One interesting finding in this study is that concussion appears to affect particular networks in the brain. These findings are in agreement with some of the typical clinical features of concussion; however, they are based on trends seen as a group. In future, the authors intend to investigate individual brain networks and develop guidelines for personalised treatment and recovery.
This story was contributed by the Florey Institute of Neuroscience and Mental Health NIF Node. For more information, please contact Shawna Farquharson or David Abbott.
More information about concussion is available here, or by speaking to your GP.